Your heart is a rhythmic organ. With its recognizable sound (“lub dub, lub dub”), it beats oxygen-rich blood to the rest of your body. While its rhythm is crucial to its functioning, many people experience something called an arrhythmia — or a problem with the rhythm of how your heart beats.
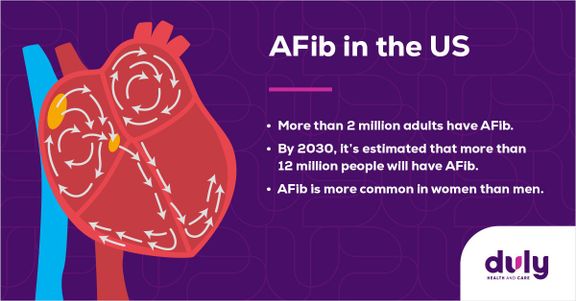
The most common type of arrhythmia is called atrial fibrillation, also known as AFib.
Source: National Heart, Lung and Blood Institute
Despite how common AFib is, it shouldn’t be ignored. This type of arrhythmia can lead to hospitalizations, heart failure, stroke, and death. Knowing the signs of AFib and how it can be prevented can save your life.
Here’s everything you should know about AFib, including how it’s diagnosed and treated.
What Exactly is Atrial Fibrillation?
Your heart has four chambers, which are the sections of your heart through which blood flows. There are two upper chambers (called the atria) and two lower chambers (called the ventricles).
In a heart that beats normally, blood starts pumping at the right atrium, passes through the right ventricle, then goes to the lungs to get oxygen. Then, it comes back to the heart, into the left atrium, and through the left ventricle. Finally, it pumps out to the rest of the body.
If you have atrial fibrillation, the beating in the left upper chamber (left atrium) is abnormal. This means that your blood doesn’t flow as it should.
AFib can happen periodically, or it can happen continuously.
Atrial Fibrillation and Stroke
AFib is a major risk factor for stroke. This is because AFib can cause blood to pool in your heart, which can lead to blood clots. About 1 in 7 strokes are caused by AFib.
A stroke related to atrial fibrillation occurs when a clot forms in the heart where atrial fibrillation is occurring (left atrium), which then moves out of the heart and possibly to the brain. Any kind of stroke can lead to brain damage, long-term disability, or death. Stroke caused by AFib is usually more severe than with other causes.
Determining if You Have AFib
Diagnosing AFib is crucial to getting the right treatment and preventing further complications. However, not only can AFib symptoms be subtle, but they can also be non-existent.
If you do experience signs of AFib, they can include:
- Heart palpitations (fluttering, rapid, or pounding heart)
- Irregular heartbeat
- Chest pain
- Extreme tiredness/fatigue
- Lightheadedness
- Shortness of breath
- Low blood pressure
- Syncope or passing out
Symptoms of AFib may occur occasionally, or they may be more frequent. As you age, AFib episodes may get longer, happen more often and can become more symptomatic.
If you think you might have atrial fibrillation, talk to your healthcare provider. Find a cardiologist near you to discuss your symptoms.
Part of knowing whether or not you have AFib centers on you paying attention to your body. If you notice any AFib symptoms, keep track of when and for how long they occur. This can help your healthcare provider identify the next steps, which may include a physical exam and a review of your family history. They may also use tests like an electrocardiogram (EKG), which measures the electrical activity in your heart, or a Holter or event monitor, a portable EKG that measures your heart’s activity as you go about your day.
With all of this information, your provider can assess your risk of AFib and potential complications, which will help determine treatment options.
How is Atrial Fibrillation Treated?
If your healthcare provider diagnoses you with AFib, there are a number of treatment options.
Treatment for AFib may include:
- Healthy lifestyle changes, such as reaching and maintaining a healthy weight, limiting alcohol, not smoking, treating possible sleep apnea and staying active
- Medications to control your heartrate, such as beta-blockers or calcium channel blockers
- Medications to control your heart’s rhythm, such as antiarrhythmic drugs
- Medications to prevent blood clots, such as blood thinners
- Outpatient procedures, such as atrial fibrillation ablation which is performed through the veins in your legs leading to your heart
- Surgery, which is typically only done to simultaneously treat another heart condition
Recognizing the Signs of an Emergency
If you do have AFib, it’s important to know that it can lead to serious complications. If you see any of the following signs of an emergency, call 9−1−1 right away:
- Stroke signs, such as a sudden headache or sudden weakness, trouble speaking, walking, or seeing
- Medication complications, such as bright red vomit, bright red blood in your stool, or blood in your urine
- Excessive bleeding or easy bruising
- Heart attack signs, such as chest pain or pressure, squeezing, or fullness in the center of your chest
- Cardiac arrest signs, such as chest pain, shortness of breath, nausea, or vomiting
Living With Atrial Fibrillation
Finding out you have a heart condition can be scary, but atrial fibrillation is a manageable condition. By staying on top of your follow-up appointments, your healthcare provider can monitor your condition, discuss how to prevent future AFib events, and review what to do in an emergency.
Together, you and your healthcare provider can have a plan to live safely with atrial fibrillation.
Health Topics: