Chances are you’ve experienced dizziness at some point in your life. That sensation of lightheadedness can be a symptom of many things — medication, heart and/or neurological conditions and head trauma. But what happens when that dizziness doesn’t go away, lasts for days and makes the room seem like it’s spinning even when you’re not moving?
It may be a sign that you’re experiencing vertigo, a vestibular dysfunction that can be a debilitating in some cases.
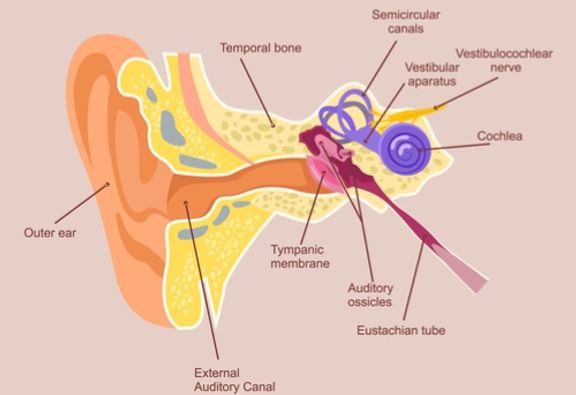
Our bodies maintain balance with sensory information from three systems: vision, proprioception (sensory receptors in the skin, muscles and joints) and the vestibular system (inner ear — provides information about motion, equilibrium and spatial orientation).
The vestibular system is located in your inner ear and made up of the utricle, saccule and three semicircular canals. When the vestibular system isn’t functioning properly, a person may experience:
- Dizziness (lightheadedness, faintness, unsteadiness)
- Vertigo (perceived movement, spinning of self or surroundings)
- Disequilibrium (unsteadiness, imbalance, disorientation)
- Spatial disorientation (not knowing where your body is in space)
- Lack of concentration
- Visual disturbance
- Hearing changes
If you’re experiencing any of these symptoms, you should see your primary care provider. You may be referred to a specialized therapist for vestibular rehabilitation therapy (VRT). Vestibular physical therapists can perform further evaluation to help determine the cause of your symptoms. They can also provide you with an individualized treatment plan to address your needs, including cases of inner ear disorders. Patients undergoing physical therapy with these conditions perform exercises that retrain the vestibular system to reduce or eliminate dizziness or imbalance related to position changes and movement.
Common Vestibular Disorders
Benign Paroxysmal Positional Vertigo (BPPV): The most common vestibular disorder is BPPV. With BPPV, otoconia (calcium carbonate crystals) located in the inner ear system are displaced from the utricle into the semicircular canal. While moving within the canal, groups of crystals can cause vertigo (room-spinning dizziness) that lasts approximately 20 – 30 seconds. This usually occurs with position change such as moving from lying to sitting, bending forward or tilting your head back. Imbalance and light headedness are also common symptoms.
There are 3 canals in which the crystals can be displaced in each ear. Your vestibular therapist can identify the canal and perform the appropriate head movements, such as the Epley maneuver, to move the crystals back into the utricle.
Vestibular neuritis/labyrinthitis: This is another common disorder caused by inflammation in the inner ear or nerves connecting the inner ear to the brain, disrupting the transmission of sensory information from the ear to the brain. Symptoms can include mild dizziness to severe room-spinning vertigo, which can occur at rest or with movement, nystagmus (abnormal movement of the eyes) which can cause problems with eye stabilization, nausea, vomiting, difficulty concentrating, unsteadiness and hearing loss (more common with labyrinthitis).
Vestibular rehabilitation can help stabilize your eyes, connect head and eye movements, improve depth perception and increase tolerance to movement in the surrounding area.
Post-concussion syndrome: Following head trauma, such as a concussion, you may experience dizziness, imbalance, headache, neck pain, whiplash, and/or difficulty concentrating. A vestibular physical therapist can assess your vestibular system, cervical spine (neck) and response to activity to identify which systems have been affected by head injury. An individualized therapy program may be planned to help you return to daily and recreational activities. This may include eye and head movement exercises, strengthening and balance exercises and manual therapy.
What to expect during your vestibular physical therapy evaluation:
A specialized physical therapist will meet with you to discuss your symptoms. Your vestibular system will then be evaluated, which includes observation of your eye movements while sitting and when moving between positions. Your evaluation may include a balance screening, muscle strength testing and observation of daily activities.
Your therapist may recommend that you attend physical therapy (PT) 1 – 2 times per week as long as your symptoms remain present, however this will be modified based on the cause of your symptoms and ability to perform exercises without PT supervision. Depending on the cause of your dizziness (for example, BPPV vs. vestibular neuritis), you may improve after 1 – 2 visits or your symptoms may slowly improve over the course of 6 – 8 weeks. Following your evaluation, your physical therapist will create an individualized a treatment plan to address your symptoms.
If you’re experiencing dizziness or spinning that impacts your daily life, see your primary care physician right away and ask if vestibular rehabilitation therapy is a treatment option for your condition. Our vestibular physical therapists can provide you with treatments to help get your world back in alignment.
Health Topics: