The Basics: What Is Glaucoma?
Glaucoma is a disease that damages the optic nerve at the back of your eye, which can lead to vision loss and blindness if left untreated.
The most common form of glaucoma is called “Primary open-angle glaucoma.” Open-angle glaucoma causes a clogged drain-like effect. Your eye doesn’t drain fluid out like it should and eye pressure starts to build up. As the pressure continues to build, it damages your optic nerve. This is painless and initially may not cause any noticeable changes to the vision. Overtime, if left untreated, this can lead to blindness.
There are a few less common types of glaucoma, including:
- Normal tension glaucoma
- This is when people show signs of glaucoma, like blind spots or damage to their optic nerve, but have normal eye pressure.
- Angle-closure glaucoma (also known as “narrow-angle” or “acute”)
- This happens when the iris (colored part of the eye) blocks the drainage of fluid from the eye, and eye pressure builds up quickly. It can cause symptoms like sudden blurred vision, severe eye pain, eye redness, headache, nausea, and vomiting. This is an emergency that requires immediate attention due to risk of blindness if it is not treated right away.
- Congenital glaucoma
- This is a rare form of glaucoma that is present from birth when a baby has a problem with their eye that stops it from draining fluid properly.
- Secondary glaucoma
- This is glaucoma that has an identifiable cause, unlike primary open-angle glaucoma. These causes may include inflammation, trauma, steroid use, diabetes, etc…
Why You Might Be at Risk for Glaucoma
Anyone can get glaucoma, but some people are more at risk than others.
Race and ethnicity can play a significant role in the likelihood of getting glaucoma. People who are Black or Hispanic are more likely than people in other ethnic groups to get glaucoma, and they’re also more likely to develop it earlier in life. Inuit and Asian people have a greater risk of getting angle-closure glaucoma.
You may also have an increased risk for glaucoma if you:
- Have a family history of glaucoma
- Have had previous eye injuries or surgeries
- Are nearsighted (increased risk for open-angle glaucoma) or farsighted (increased risk for closed-angle glaucoma)
- Have high eye pressure
- Use corticosteroids on a long-term basis
- Have diabetes
- Are over age 40
Why Early Diagnosis Is Key
There is no cure for glaucoma. Any damage that is present is permanent and cannot be reversed. However, there are treatments like medications, surgery, and laser therapy to help slow down or prevent vision loss. These treatments are especially effective if you start them when you’re still in the early stages of glaucoma before your vision has been too impaired.
But, there’s a catch – it can be difficult to detect glaucoma at those early stages. Vision loss from glaucoma comes on gradually and often doesn’t cause symptoms until it has become more advanced.
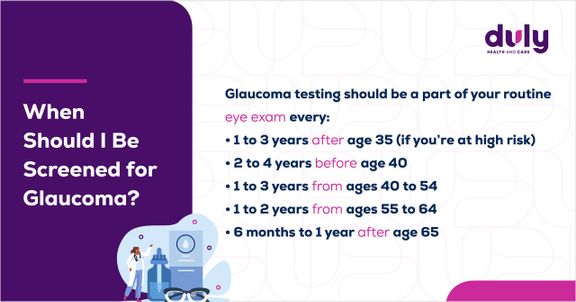
That’s why it’s so important to get regular vision tests, rather than relying solely on how well you can see, to monitor your eye health. Your provider can look for signs of damage to your optic nerve or high eye pressure that could indicate glaucoma before you even notice any vision changes.
Once you’ve started treatment, there are also certain lifestyle modifications you can make to prevent further vision loss. Controlling your blood pressure, remaining physically active, avoiding smoking, cutting back on caffeine, and keeping a healthy weight can help you control your eye pressure and improve your eye health.
By taking care of yourself and keeping up with your prescribed treatment plan, you can slow or halt glaucoma in its tracks. You’ll see.
Health Topics:








