You wake up with a headache. You got a full eight hours of sleep, but it seems impossible to stay awake during the day. You’ve always been a light snorer, but recently your snoring has been disruptive to your sleep partner.
It’s normal to have days where you feel tired or nights of heavy snoring while you fight off a cold or celebrated too much. But when they are happening frequently, it could be a sign of a disorder called sleep apnea.
Sleep apnea is a disorder that causes you to temporarily stop breathing while asleep. The most common form of sleep apnea is called obstructive sleep apnea (OSA). It happens when there’s a problem with your airway and the muscles in your throat can’t keep your airway open while you sleep. As your airway closes, oxygen levels in your blood may drop. The combination of this can lead to disruptions in your sleep, sometimes even full awakenings.
Anything that can narrow or block your upper airway may increase your risk for OSA. The most common risk factor is obesity. However, structural abnormalities that affect the throat, smoking, medicines and medical conditions, and older age may also impact your airway. Since men have a higher risk for OSA than women, it used to be thought of as a “male” disease. But that doesn’t tell the whole story.
As awareness of sleep apnea in women has grown, more women are getting tested. Here are several reasons why – and what you can do if you have sleep apnea and snore.
Increased Recognition That Symptoms of OSA May Look Different in Women
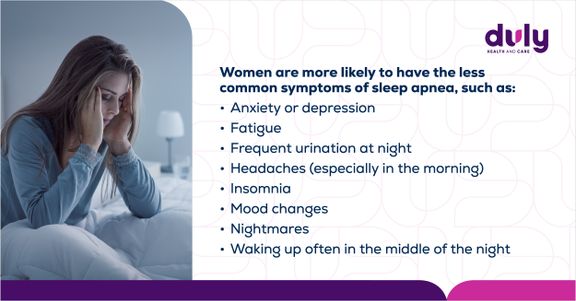
OSA is underdiagnosed in both men and women, but more so in women. One of the main reasons is that women’s symptoms aren’t always as obvious. Some symptoms are the same across the board, such as the telltale loud snoring, visibly not breathing at certain points during sleep, daytime tiredness, and snorting, gasping, or choking while sleeping. But there are some symptoms that are less common in men.
Awareness of OSA and Women’s Health Issues
Pregnancy and OSA
When you’re pregnant, the structure and function of your throat can be affected. There can also be changes in the hormones that affect breathing. These changes can increase your risk of developing OSA or make existing sleep apnea worse.
OSA during pregnancy can contribute to (or make worse) complications like high blood pressure, gestational diabetes (diabetes that occurs only during pregnancy), and other pregnancy issues.
There is good news. Many sleep apnea treatments (like CPAP machines) are safe to use during pregnancy, and treating OSA during pregnancy can lower the risk of complications. And, while sleep apnea doesn’t always disappear after giving birth, the symptoms often improve.
A Word From Our Provider
“I try to impress upon patients that your sleep is essential for good health and a good quality of life. Testing is easily obtained and we can do much testing in the comfort of your home these days. I would like to emphasize that CPAP is very effective and much easier to tolerate compared to the past.
I have many patients who could not tolerate CPAP 15 years ago and found it cumbersome, who when treated with new CPAP machines with new masks, found it to be much improved and easier tolerated. There are better alternatives than what we had in the past.
Ultimately, one of the most important things we do is help patients feel confident and comfortable about their health and care.”
– Dr. Ravi Nemivant, MD, Sleep medicine physician at Duly Health and Care
Ready to reclaim your energy and sleep soundly again? Our Sleep Medicine team at Duly Health and Care offers comprehensive testing and treatment options right here in your community. Call to schedule an appointment with a sleep specialist to explore solutions tailored to you.
Find sleep medicine providers near you >
Menopause and OSA
After menopause, loss of reproductive hormones like progesterone and estrogen can increase your risk of OSA. Postmenopausal women are two to three times more likely than premenopausal women to develop sleep apnea.
OSA that begins during or after menopause is easy to miss, since many of the symptoms of OSA and menopause overlap. If you’re having symptoms like daytime sleepiness, trouble sleeping, or increased snoring, let your provider know.
Polycystic Ovary Syndrome (PCOS) and OSA
PCOS is a condition that affects hormones during reproductive years, and it increases your risk of developing other medical conditions, including OSA. One reason is that PCOS can lead to problems like weight gain and obesity. PCOS can cause multiple hormonal changes that can effect sleep quality and increase the risk for sleep apnea.
Also read: Polycystic Ovary Syndrome: What to Expect From PCOS
What to Do If You Snore: Treatment for OSA
Whether your snoring is thundering across the house or just barely noticeable, it’s critical to get treated for OSA. If it’s not managed, OSA can lead to significant complications, like glucose intolerance and metabolic syndrome, high blood pressure, and in severe cases, untreated sleep apnea can increase the risk of stroke, heart rhythm changes and possibly cardiovascular events. Lack of treatment of OSA can also lead to worsening control of cardiac conditions like heart failure.
Also, even if you don’t snore, OSA can cause excessive daytime sleepiness. This can put you in dangerous situations, like falling asleep behind the wheel or while operating machinery.
Treatment is generally the same for both women and men. One of the most common and the most effective treatments for OSA is a continuous positive airway pressure (CPAP) machine, which keeps your airway open while you sleep. CPAP has become much more comfortable and easier to tolerate with the various masks and with how the machines currently function. There are other ways to treat OSA, including:
- Inspire®: A small device implanted under the skin of your chest connected to wires implanted in the muscles around the throat that prevents the muscles from relaxing and keeps your airway open while you sleep.
- Oral appliance: A mouthpiece you wear during sleep that pulls your jaw and tongue forward to open your airway.
- Lifestyle changes: Losing weight, quitting smoking, limiting alcohol use, avoiding sleeping pills, or sleeping on your side.
- Zepbound® (tirzepatide): Injectable weight loss medication recently approved for treating moderate to severe OSA.
- Surgery: Procedures like removing soft tissue in your throat or adjusting your jaw to address the structural causes of OSA. Additionally, the weight loss experienced through bariatric surgery can help to treat sleep apnea .
Also read: Inspire, a New Treatment for Obstructive Sleep Apnea
If you have symptoms like daytime sleepiness, insomnia, waking up in the middle of the night gasping for breath, or loud snoring, talk to your provider.
They may recommend getting a sleep study to test for sleep apnea, and they can help you find ways to get the sleep you need.








